Transforming Appeals & Grievances
Quality improvement is talked about more and more across the healthcare ecosystem. Quality isn’t just the service provided, but the complete process of doing business. Managing the appeals and grievances process is not only about quick and accurate resolutions, but the quality of service when coming to a decision.
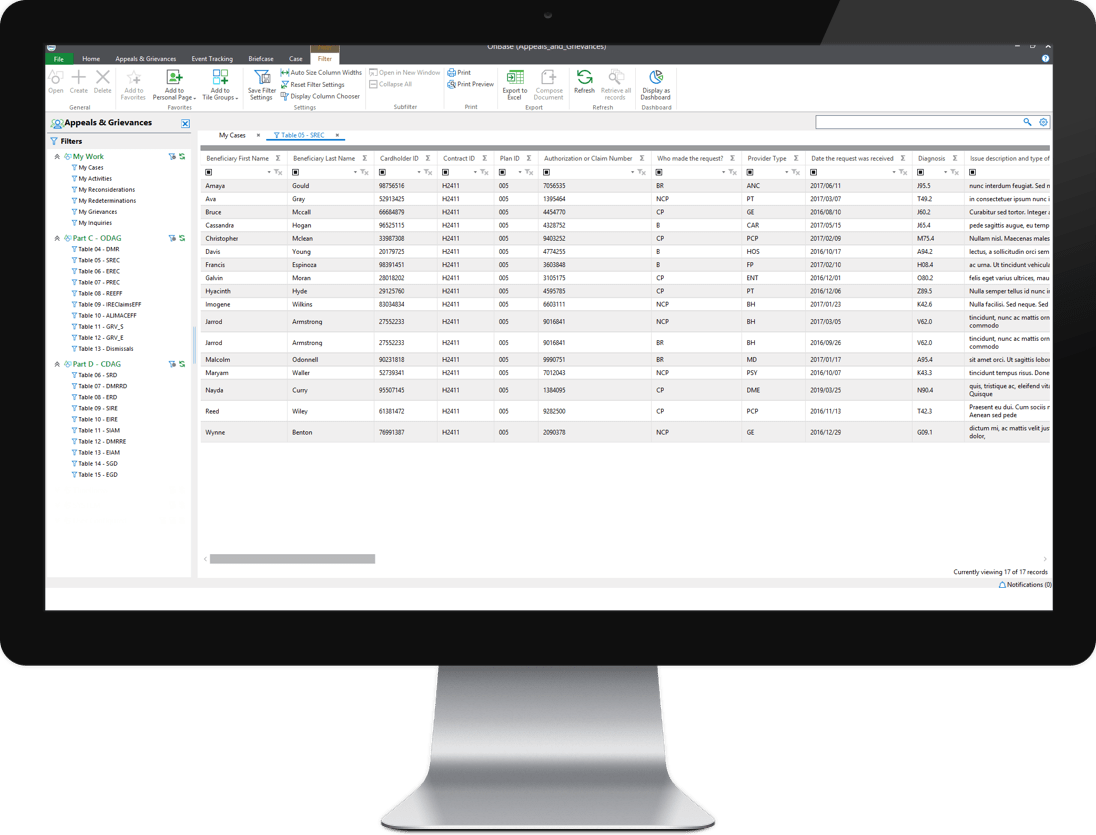
Kiriworks Appeals & Grievances (A&G) helps healthcare payers improve compliance, increase productivity, improve quality scores and boost member and provider satisfaction. Whether Medicare, Medicaid or commercial, the solution streamlines the appeals and grievances life cycle through automated processing, communication and reporting. Business rules are built on a plan’s (or state’s) regulatory requirements and guidelines. Cases are all prioritized based off a standard or expedited appeal or grievance and each stage of the process documents all internal and external communications. Universe reports are generated by the click of a mouse and additional reporting allows management greater process insight.
Features
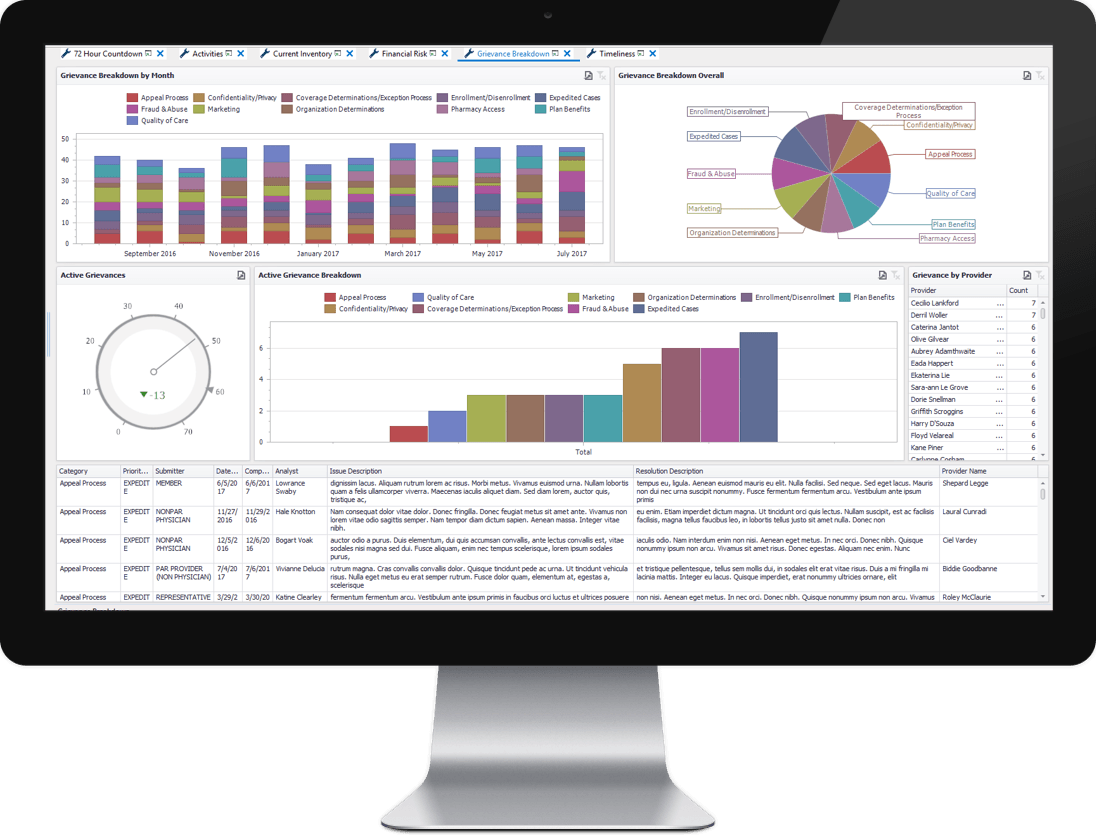
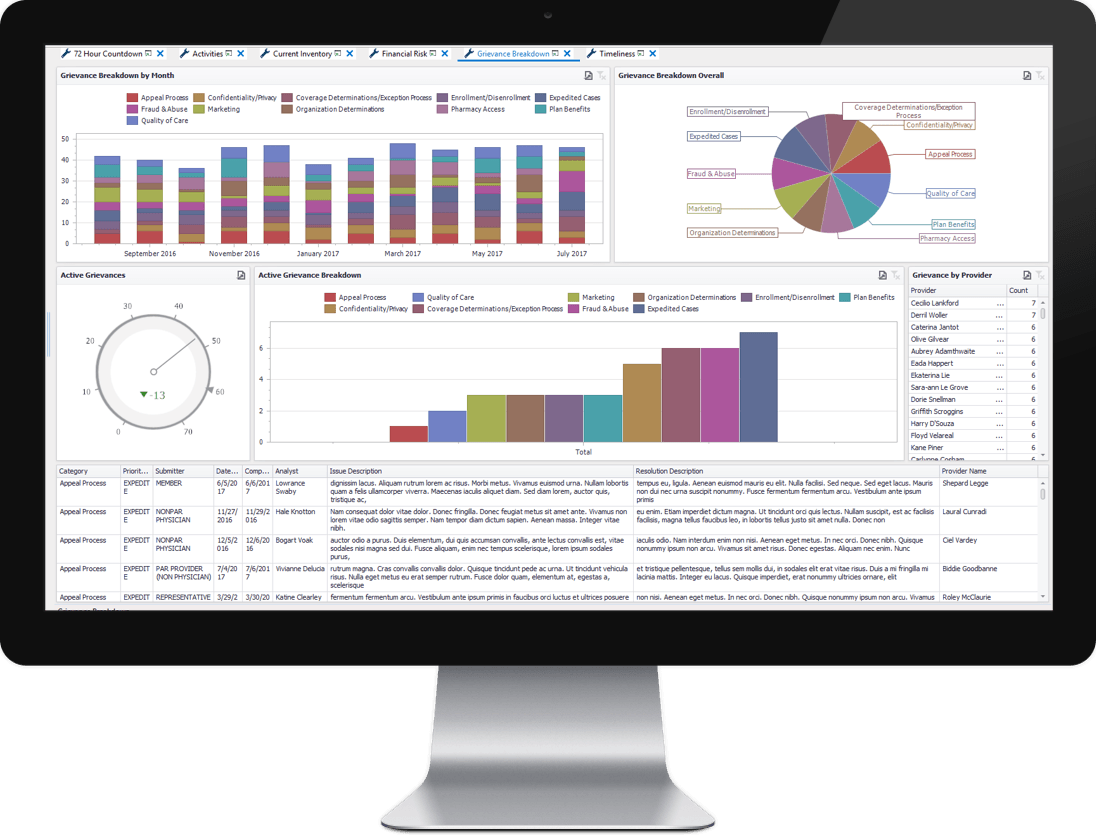
Reporting Dashboards
Kiriworks A&G comes out of the box with 7 standard dashboard reports that provide real-time business insights about a payer’s appeals and grievances operations. From monitoring financial risk to inventory management – Kiriworks A&G delivers actionable business intelligence.
- Visual alerts to ensure case compliance
- Fully customizable by business users
- Cases can be accessed directly from dashboards
- Real-time filtering and splicing of data
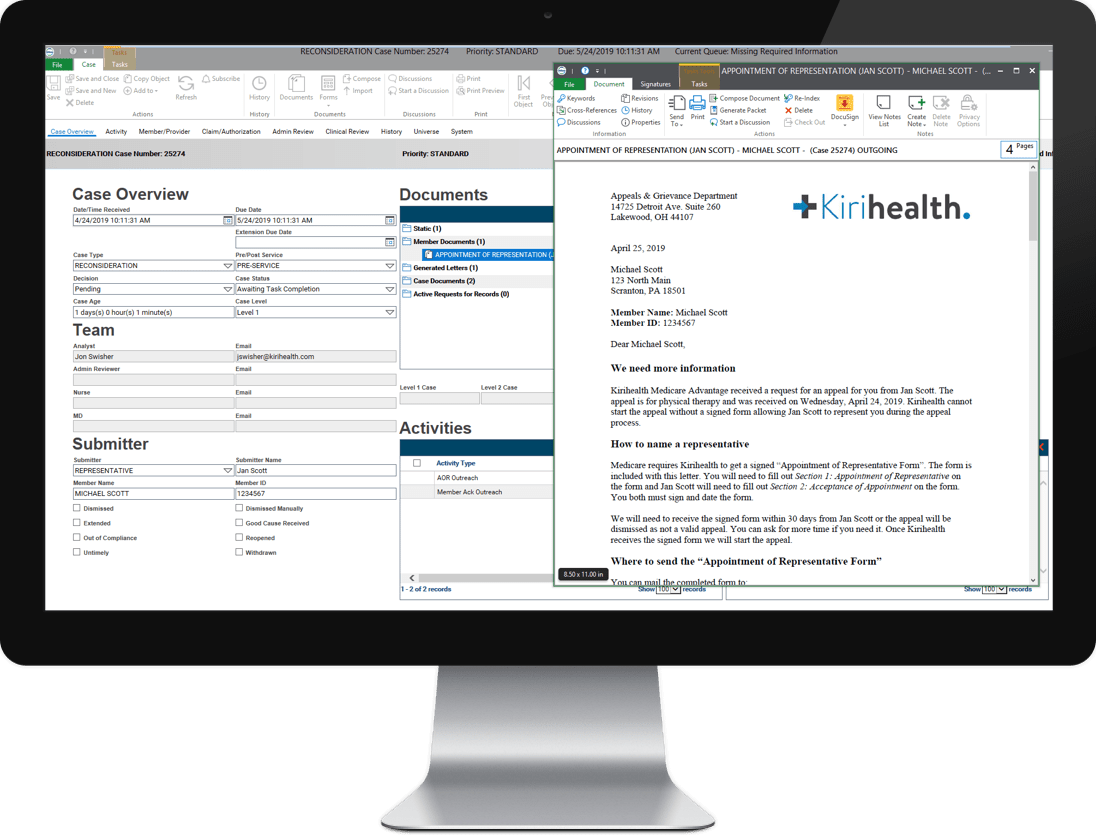
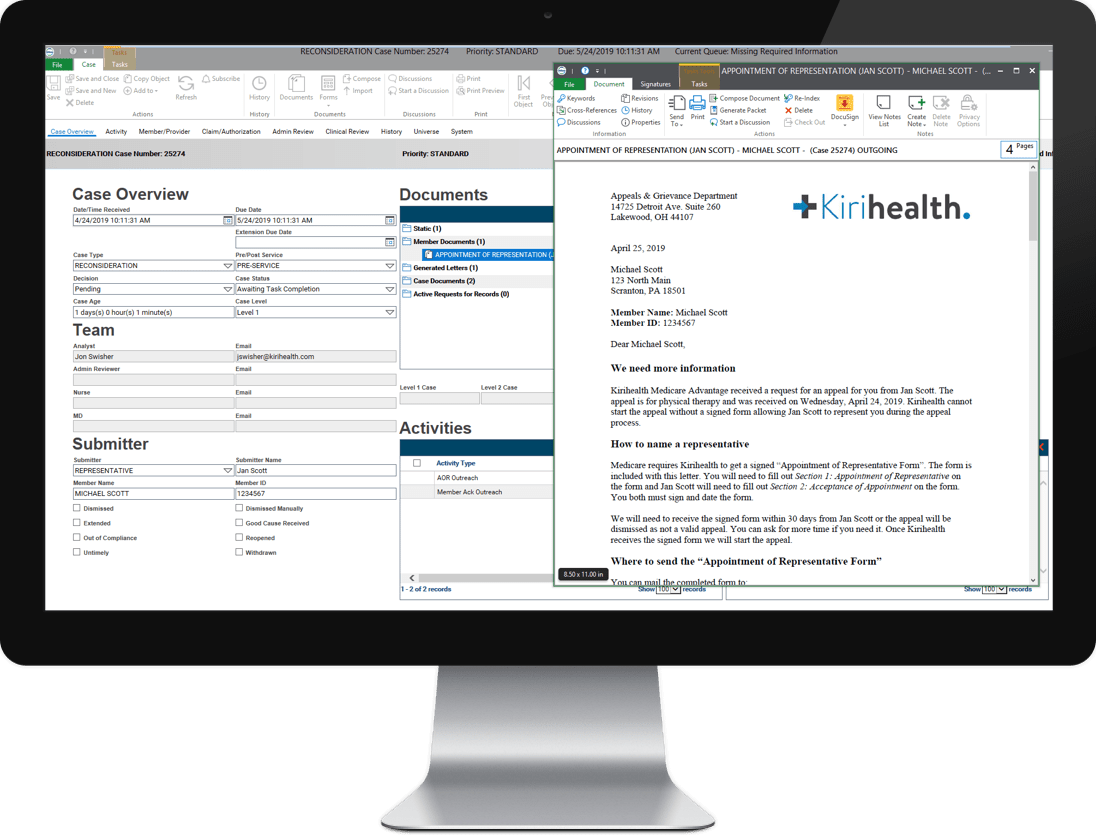
Automated Correspondence
Timely and accurate correspondence with members, providers and representatives is vital to the quality of a payer’s appeals and grievances operations. Kiriworks A&G generates the right letter, at the right time, with the right language helping payers meet their quality standards.
- One central location for all correspondence templates
- Letters automatically selected based on process stage
- Case-based dynamic correspondence content
- Plan or LOB specific content or design (letterhead, logos, etc.)
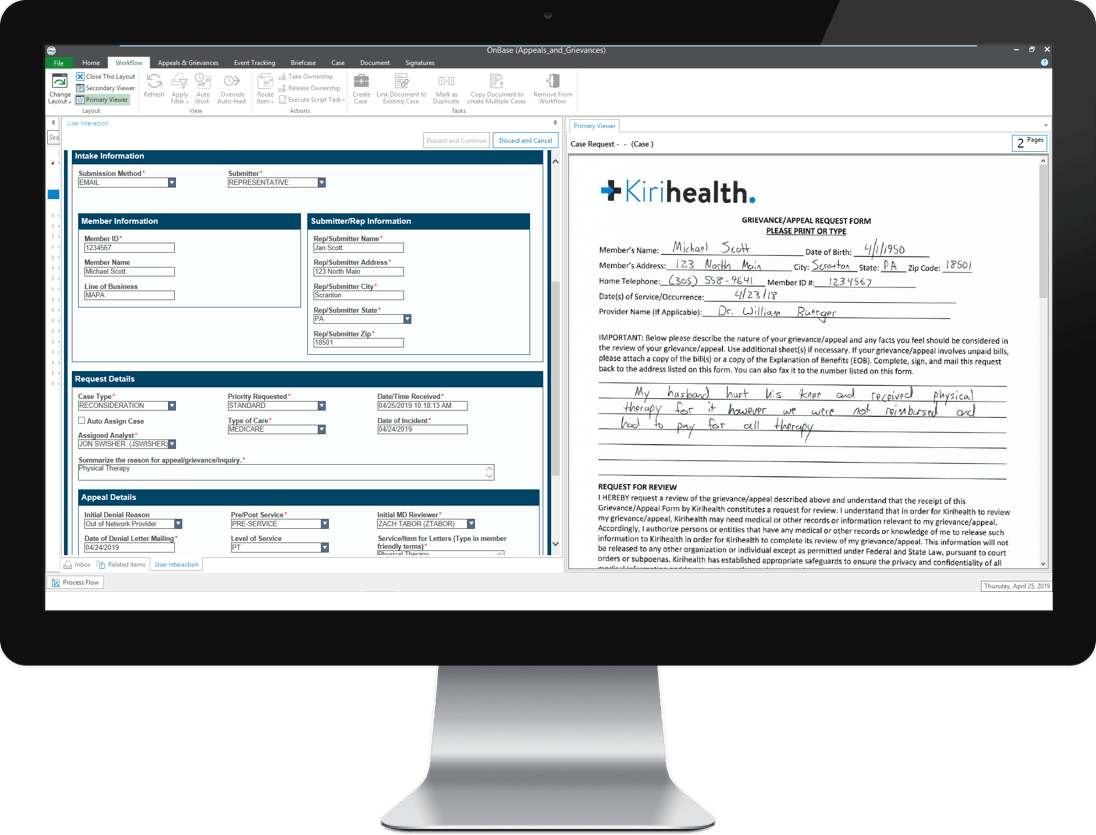
Multiple Intake Methods
Kiriworks A&G has been designed to intake case requests from various methods including email, fax, mail, phone or online portal. The solution delivers an intelligent classification process that aides end users in correctly selecting the appropriate case type and capture the required information at the time of case creation.
- Intelligent, rules-driven case intake process
- Auto-classification of case types by LOB
- Integrate with Member Service applications like Salesforce
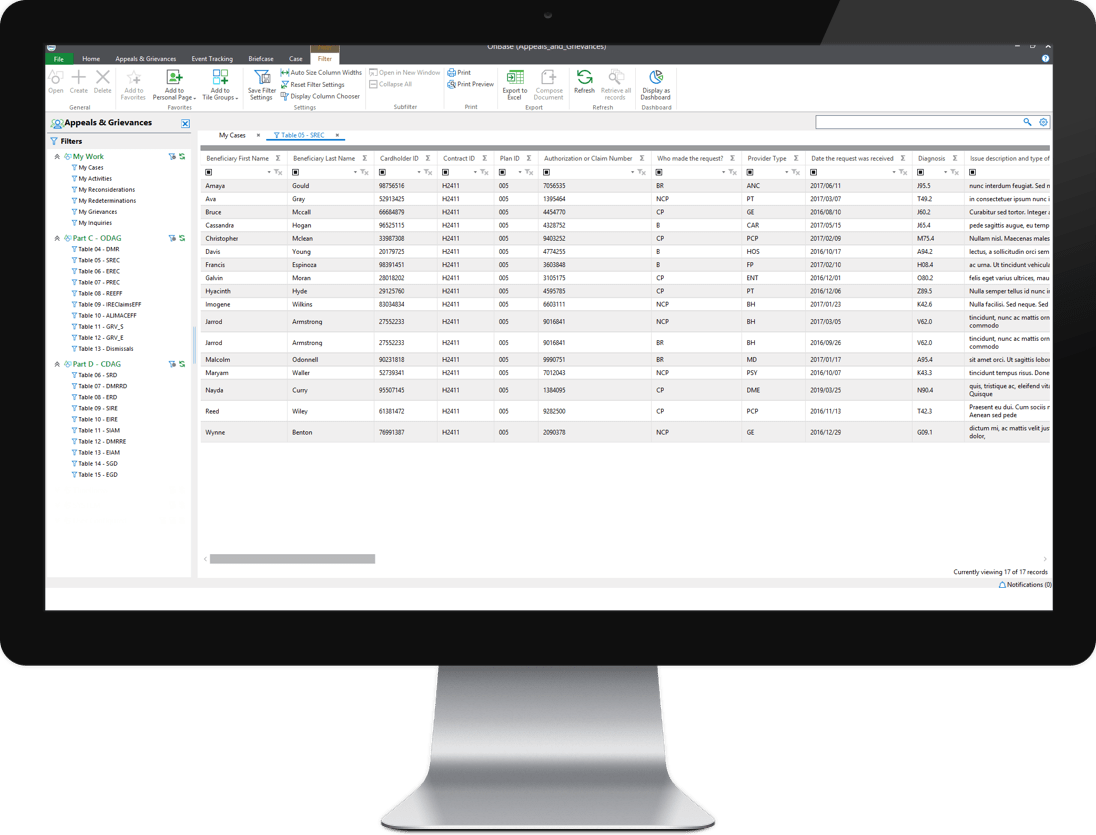
Regulatory Reporting
Kiriworks A&G for Medicare enables users to create regulatory reports like ODAG and CDAG universes with a single mouse click. This same foundation allows business users to create custom reports to surface any piece of data created by or accessed by the case. Whether it is pre-built regulatory reports or customer reporting needs – Kiriworks A&G has the right tools.
- ODAG & CDAG Universes and Timeliness Monitoring
- Quarterly Data Submissions for CMS
- Wizard-driven customer reporting interface
-
Medicare
Universe: Pre-built CMS Universe tables that are automatically populated. Tables are easily searchable and can be exported to excel with the click of a mouse.
Compliance: Helps adhere to CMS compliance deadlines and regulatory requirements along with intelligently requesting proper documentation throughout the appeals & grievances process.
Data Submission: Ability to create and store quarterly data validation reports for annual submission. Easing the administration of reporting and audit preparation.
-
Universal A&G for Medicaid and Commercial payers
Regulations: Configurable to federal and state regulatory requirements. Ability to use multiple Independent Review Organizations and designate the pattern in which appeals get assigned.
Flexibility: Set individualized rules and activities per plan and/or state. Easily change and administer how cases are managed and processed. Modify rules, process guidance, SLAs and reports.
Reporting: Ability to customize reports based on plan and/or state guidelines with specific classification and terminology, plan and plan level specific activities such as verbal acknowledgements, automatic extensions and/or priority review.
Benefits
-
Maintain Compliance
Adhere to compliance deadlines and regulatory guidelines to ensure timeliness of resolution and avoid fines and penalties.
-
Timely Resolutions
Automated processing ensures timeframes of standard and expedited cases are managed correctly.
-
Central Repository
Leverage existing member and claim data for real-time processing of cases.
-
Process Visibility
Leverage dashboards to manage all cases, keep managers informed and avoiding bottlenecks within the process.
-
Real Time Monitoring
Provides holistic view into expedited cases and automatically notifies correct parties of approaching due dates.
-
Improve Member Satisfaction
Ensure members are provided the correct correspondence and notified in a timely manner of all decisions.
DISCLAIMER: While Kiriworks healthcare payer accelerator products are designed to aid in the collection, management and reporting of business content, these products do not relieve users of responsibility to insure compliance with all applicable state and federal regulations and implement procedures to examine and verify for completeness and accuracy of all data and output before its use.